Leads ECG Placement: 7 Critical Mistakes You Must Avoid Now
Understanding the correct leads ecg placement is essential for accurate cardiac diagnostics. A misplaced electrode can lead to misdiagnosis, delayed treatment, or unnecessary testing. In this comprehensive guide, we’ll break down everything you need to know about proper ECG lead positioning, common errors, and best practices used by healthcare professionals worldwide.
What Is Leads ECG Placement and Why It Matters

Leads ecg placement refers to the precise positioning of electrodes on the body to record the heart’s electrical activity. An electrocardiogram (ECG or EKG) uses 12 different leads derived from 10 electrodes placed on the limbs and chest. These leads provide a comprehensive view of the heart’s function from multiple angles.
The Science Behind ECG Leads
Each lead in an ECG represents a specific electrical vector through the heart. The standard 12-lead ECG includes three types of leads: limb leads (I, II, III), augmented limb leads (aVR, aVL, aVF), and precordial (chest) leads (V1–V6). Proper leads ecg placement ensures that each of these vectors is accurately captured.
- Limb leads measure electrical activity in the frontal plane.
- Precordial leads assess the horizontal plane, focusing on the left ventricle.
- Incorrect placement distorts these vectors, leading to inaccurate readings.
“A 12-lead ECG is only as good as the electrode placement,” says Dr. Richard Chazal, former president of the American College of Cardiology.
Clinical Impact of Improper Placement
Misplaced leads can mimic or mask serious cardiac conditions such as myocardial infarction, arrhythmias, or bundle branch blocks. For example, reversing the right and left arm electrodes can create a pattern resembling dextrocardia or lead to misinterpretation of ST-segment changes.
A study published in the Journal of Electrocardiology found that up to 40% of ECGs in clinical settings have some degree of lead misplacement, significantly affecting diagnostic accuracy.
Step-by-Step Guide to Correct Leads ECG Placement
Accurate leads ecg placement follows standardized guidelines established by organizations like the American Heart Association (AHA) and the Association for the Advancement of Medical Instrumentation (AAMI). Following these steps meticulously ensures reliable results.
Preparing the Patient and Equipment
Before placing any electrodes, proper patient preparation is crucial. The patient should lie flat, relaxed, with arms at their sides and legs uncrossed to minimize electrical interference.
- Clean the skin with alcohol wipes to remove oils and dead skin cells.
- Shave excessive chest hair if necessary to ensure good electrode adhesion.
- Ensure the room is warm and quiet to prevent shivering or muscle tremors that can distort the tracing.
Placing Limb Electrodes Correctly
The four limb electrodes are placed on the wrists and ankles, not directly on the limbs themselves. According to AAMI standards:
- RA (Right Arm): On the right forearm, near the wrist.
- LA (Left Arm): On the left forearm, near the wrist.
- RL (Right Leg): On the right lower leg, near the ankle (ground electrode).
- LL (Left Leg): On the left lower leg, near the ankle.
These placements minimize motion artifacts and ensure consistent signal acquisition. Avoid placing electrodes over bony prominences or large muscles to reduce noise.
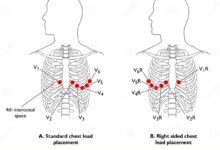
Positioning the Chest (Precordial) Leads
The six precordial leads (V1–V6) are placed in specific intercostal spaces across the chest. This is where most errors in leads ecg placement occur.
- V1: 4th intercostal space, right sternal border.
- V2: 4th intercostal space, left sternal border.
- V3: Midway between V2 and V4.
- V4: 5th intercostal space, midclavicular line.
- V5: Same horizontal level as V4, anterior axillary line.
- V6: Same level as V4 and V5, midaxillary line.
Accurate identification of anatomical landmarks is critical. Misplacement of V1 and V2 by just one intercostal space can alter R-wave progression and mimic anterior infarction.
Common Errors in Leads ECG Placement and How to Fix Them
Even experienced clinicians can make mistakes in leads ecg placement. Recognizing and correcting these errors is vital for diagnostic precision.
Reversed Limb Electrodes
One of the most frequent errors is switching the right and left arm electrodes. This causes lead I to invert, and leads II and III to swap. The result? A false appearance of dextrocardia or limb lead reversal patterns.
- Symptoms: Negative P, QRS, and T waves in lead I.
- Solution: Always double-check RA and LA placement before starting the recording.
- Tip: Use color-coded cables (White = Right, Black = Left, Red = Right Leg, Green = Left Leg) as a visual aid.
Incorrect Chest Lead Positioning
Placing V1 too high or too low is a common mistake. Similarly, V4 placement outside the 5th intercostal space can distort the QRS complex and ST segments.
A study in The American Journal of Emergency Medicine showed that 30% of emergency department ECGs had at least one precordial lead misplaced, often leading to misdiagnosis of ischemia.
- Fix: Use anatomical landmarks consistently. Palpate the angle of Louis (sternal angle) to locate the 2nd rib, then count down to the 4th intercostal space.
- For women, place V4–V6 at the level of the nipple line, not under the breast.
Failure to Identify Anatomical Variants
Patient anatomy varies—obesity, breast tissue, surgical scars, or barrel chests can obscure landmarks. In such cases, standard leads ecg placement may need adjustment.
- For large-breasted patients, lift the breast to place V3–V6 on the chest wall, not on the breast tissue.
- In patients with kyphoscoliosis, consider modified lead placement or use of alternative ECG systems.
- Document any deviations from standard placement in the patient’s record.
Special Considerations for Leads ECG Placement in Different Populations
While standard guidelines apply to most adults, special populations require tailored approaches to ensure accurate leads ecg placement.
ECG in Pediatric Patients
Children have smaller thoraxes and different heart positions, making standard adult lead placement unsuitable.
- Use smaller electrodes designed for pediatric use.
- Place precordial leads based on anatomical landmarks, not age-based formulas.
- V4 placement remains at the 5th intercostal space, midclavicular line, regardless of age.
The American Academy of Pediatrics recommends using pediatric ECG interpretation criteria due to normal variations in heart rate and axis.
Leads ECG Placement in Obese and Elderly Patients
Obesity can make it difficult to locate intercostal spaces, while elderly patients may have skin fragility or reduced muscle mass affecting signal quality.
- Use extra pressure when palpating to feel rib spaces through adipose tissue.
- Consider using gel-based electrodes for better conduction in dry or fragile skin.
- Ensure the patient is supine and relaxed to avoid diaphragmatic shift.
ECG in Pregnant Women
Pregnancy alters cardiac position and diaphragmatic elevation, which can shift the precordial leads upward.
- Place V1 and V2 in the 3rd or 4th intercostal space depending on diaphragmatic rise.
- V4–V6 may need to be placed higher than usual, especially in the third trimester.
- Always note pregnancy status on the ECG report for accurate interpretation.
Technological Advances Improving Leads ECG Placement Accuracy
Modern technology is helping reduce human error in leads ecg placement through innovative tools and systems.
Digital ECG Systems with Real-Time Feedback
Newer ECG machines now include real-time impedance monitoring and lead placement verification. These systems alert technicians if an electrode is not making proper contact or if lead reversal is detected.
- Philips ECG machines feature “Lead Check” technology that identifies reversals instantly.
- GE Healthcare’s MAC 1200 provides visual guides on screen for correct lead placement.
- These tools reduce repeat tests and improve workflow efficiency.
Wearable ECG Monitors and AI Integration
Devices like the Apple Watch ECG and AliveCor KardiaMobile allow single-lead recordings, but they don’t replace the 12-lead standard. However, AI algorithms are being developed to detect lead misplacement in traditional ECGs.
Researchers at Stanford University have trained machine learning models to identify limb lead reversals with over 95% accuracy by analyzing waveform patterns.
- AI can flag potential errors before the ECG is interpreted by a physician.
- Future systems may auto-correct for minor placement deviations.
- Integration with electronic health records (EHR) enhances data consistency.
3D Body Mapping for Precision Placement
Experimental systems use 3D scanning to map the patient’s torso and guide optimal electrode placement. This is particularly useful in research and complex cases.
- Reduces inter-operator variability.
- Ensures reproducibility in serial ECGs.
- Potential for use in telemedicine and remote diagnostics.
Training and Education: Building Competence in Leads ECG Placement
Despite its routine nature, leads ecg placement is often taught inadequately in medical and nursing programs. Ongoing training is essential for maintaining high standards.
Standardized Training Protocols
Hospitals and clinics should implement mandatory ECG competency assessments for all staff involved in ECG acquisition.
- Include hands-on practice with mannequins and real patients.
- Use checklists to ensure all steps are followed.
- Incorporate video tutorials and anatomical diagrams in training modules.
Certification and Continuing Education
Organizations like the National Healthcareer Association (NHA) offer ECG technician certification (CET) that includes lead placement as a core component.
- Certification ensures baseline competency.
- Continuing education units (CEUs) help maintain skills over time.
- Regular audits of ECG quality can identify training gaps.
Simulation-Based Learning
Medical schools and nursing programs are increasingly using simulation labs to teach ECG skills.
- Students practice on high-fidelity mannequins with realistic anatomy.
- Instructors can simulate lead reversals and challenge students to detect them.
- Immediate feedback reinforces correct technique.
Legal and Ethical Implications of Incorrect Leads ECG Placement
Misplaced leads aren’t just a technical issue—they can have serious legal and ethical consequences.
Diagnostic Errors and Patient Harm
An incorrectly placed ECG can lead to false positives (unnecessary interventions) or false negatives (missed heart attacks). Both scenarios expose healthcare providers to malpractice risks.
- Example: A reversed limb lead mimicking ST elevation could lead to unnecessary thrombolytic therapy.
- Conversely, a missed anterior infarction due to misplaced V1–V2 can delay life-saving intervention.
- Documentation of proper technique can serve as a legal defense.
Documentation and Accountability
Every ECG should include a notation of lead placement, technician name, and any deviations from standard protocol.
- This transparency supports quality assurance.
- Facilitates peer review and error analysis.
- Meets Joint Commission and CMS requirements for patient safety.
Professional Responsibility
Healthcare providers have an ethical duty to perform ECGs correctly. This includes staying updated on best practices and seeking help when uncertain.
- Admitting uncertainty is better than risking patient harm.
- Peer mentoring and supervision can reduce errors.
- Creating a culture of safety encourages reporting of near-misses.
Best Practices Summary for Flawless Leads ECG Placement
To ensure the highest quality ECG recordings, follow these evidence-based best practices for leads ecg placement.
Pre-Procedure Checklist
Verify patient identity and indication for ECG.Explain the procedure to the patient to reduce anxiety.Ensure the patient is lying flat, warm, and still.Check equipment functionality and electrode supply.During Procedure Protocol
Palpate anatomical landmarks before placing any electrode.Use alcohol wipes to clean skin; shave if needed.Follow the RA, LA, RL, LL, V1–V6 sequence systematically..
Confirm cable connections match electrode sites.Run a quick lead check before final recording.Post-Procedure Review
Inspect the ECG tracing for signs of lead reversal or artifact.Document any non-standard placement in the report.Label the ECG with patient name, date, time, and technician.Archive the ECG in the medical record securely.What happens if ECG leads are placed incorrectly?.
Incorrect leads ecg placement can lead to misdiagnosis, such as false signs of myocardial infarction, arrhythmias, or chamber enlargement. It may also mask real cardiac abnormalities, delaying critical treatment. Common errors include limb lead reversals and misplaced precordial leads.
How can I verify correct ECG lead placement?
You can verify correct leads ecg placement by checking for expected waveform patterns: upright P waves in lead II, progressive R-wave progression from V1 to V6, and consistent QRS morphology across leads. Modern ECG machines often include real-time lead verification alerts.
Are there alternatives to standard 12-lead ECG placement?
Yes, in certain cases like dextrocardia or post-surgical patients, modified lead placement (e.g., right-sided or posterior leads) may be used. However, these should be clearly documented and interpreted by experienced clinicians.
Can AI detect ECG lead misplacement?
Yes, emerging AI systems can analyze ECG waveforms to detect common errors like limb lead reversals or misplaced precordial leads. These tools are being integrated into digital ECG systems to improve accuracy and reduce human error.
How often should ECG technicians be retrained?
ECG technicians should undergo competency assessment at least annually. Regular refresher courses, simulation training, and quality audits help maintain high standards in leads ecg placement.
Accurate leads ecg placement is not just a technical step—it’s a cornerstone of reliable cardiac diagnosis. From proper limb and chest electrode positioning to understanding anatomical variations and leveraging technology, every detail matters. By following standardized protocols, engaging in continuous education, and embracing innovation, healthcare providers can ensure that every ECG delivers trustworthy, life-saving data. Remember, precision in placement means precision in care.
Further Reading: